Crohn's Disease vs. Ulcerative Colitis: What's the Difference?
October 15, 2024
Categories: Digestive Health
 By Dejan Micic, MD, Digestive Health Program
By Dejan Micic, MD, Digestive Health Program
There are nearly three million patients with inflammatory bowel disease (IBD) in the United States. Even with so many people affected, there is still confusion about what exactly IBD is, its subtypes and how to manage the disease.
What is inflammatory bowel disease?
Crohn’s disease and ulcerative colitis (UC) are the most common subtypes of inflammatory bowel disease, a group of chronic inflammatory disorders of the digestive tract.
Both Crohn’s disease and UC cause intestinal damage due to an exaggerated immune response. This immune response results in the damage of the underlying healthy cells involved in gastrointestinal digestion and absorption leading to persistent and chronic gastrointestinal symptoms. While Crohn's disease and ulcerative colitis are very similar, there are some key differences between the two.
Key differences between Crohn's and ulcerative colitis
Areas affected
- Crohn’s disease: Essentially the entire gastrointestinal tract can be impacted from the mouth to the rectum. Most commonly the end of the small intestine is inflamed.
- Ulcerative colitis: Variable extension through the large intestine.
Inflammation
- Crohn’s disease: Inflammation impacting layers of the intestinal wall.
- Ulcerative colitis: Only on the most superficial layer of the colon.
The transmural inflammation in Crohn’s disease can result in strictures (narrowing) of the intestines and abnormal connections through the weakened walls of the intestine and even the anus due to ongoing damage.
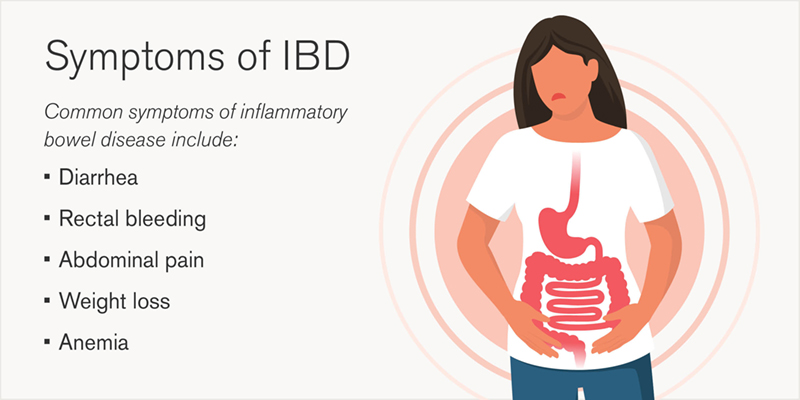
Patients with IBD may experience issues with other organ systems as well, including joint inflammation, eye inflammation or even skin disorders. These conditions are often related to IBD itself and can worsen during an IBD flare-up.
Risk factors for IBD
Patients with IBD may be at higher risk of developing other autoimmune conditions including thyroiditis, liver inflammation (primary sclerosing cholangitis) or psoriasis.
Risk factors for IBD include smoking, a family history of IBD and living in urban or northern climates.
IBD patients (even when young) are at higher risk for colon cancer after having had persistent disease that affects their colon.
For these IBD patients, in addition to effective medical treatment, a high-definition colonoscopy with targeted biopsies performed by the experienced gastroenterologists at Loyola can reduce this risk of colon cancer.
Diagnosis of IBD
While blood and stool tests can often detect subtle inflammation, the most important first test for inflammatory bowel disease is a colonoscopy (with intestinal biopsies) to look for signs of chronic inflammation. Other tests include CT scan or MRI scans or a video capsule endoscopy to specifically assess for inflammation in the small intestine.
There is no cure for IBD, but well-timed, safe and effective treatments can induce and maintain long lasting remission of the disease, thus decreasing long-term disease complications.
Treatment options for IBD
Effective treatment depends on the patient’s disease severity and location of involvement of IBD.
- First step: Anti-inflammatory medications can be an effective initial step to treat mild colon inflammation.
- Short-term: Steroids can be used as a short-term bridge to effective long-term therapy as the disease progresses.
- Long-term: Immune-suppressing medications are effective in the long-term treatment of moderate to severe IBD targeting the exaggerated immune responses often seen in IBD.
Sometimes an operation may also be needed as part of the management plan. If an operation becomes necessary, the inflammatory bowel disease team at Loyola Medicine will work together and discuss surgical options, including less-invasive laparoscopic approaches to remove parts of the affected colon or small intestine.
Find effective and personalized IBD care at Loyola Medicine
At Loyola, an ongoing personalized care plan (including the latest biologic and small molecule therapies for those that need it) is developed for each patient to address multiple aspects of disease management.
Multidisciplinary care management allows us to deliver efficient medical and surgical care while also addressing the often overlooked impact of diet on disease course.. We use proven health maintenance strategies and preventive care, as well as ongoing assessments to relate health to quality of life.
We also offer a unique Behavioral Medicine program to address the impact of stress/anxiety and how to cope with this chronic illness. Loyola’s IBD team offers a 24/7 inpatient IBD consultative service at Loyola University Medical Center, ensuring the IBD team is available when patients need us the most.
Please contact your physician for a referral if you have any concerns or symptoms of IBD.
Dejan Micic, MD, is the Associate Chief of the Division of Gastroenterology at Loyola University Medical Center. His clinical expertise includes the management of inflammatory bowel disease (IBD), adult clinical nutrition and small bowel disorders. After completing a clinical fellowship in gastroenterology at the University of Chicago, Dr. Micic underwent advanced training at Northwestern University, specializing in nutrition support.
Book an appointment today to see Dr. Micic or another Loyola specialist by self-scheduling an in-person or virtual appointment using myLoyola.
