How Your Brain and Emotions Control Your Gut
July 5, 2017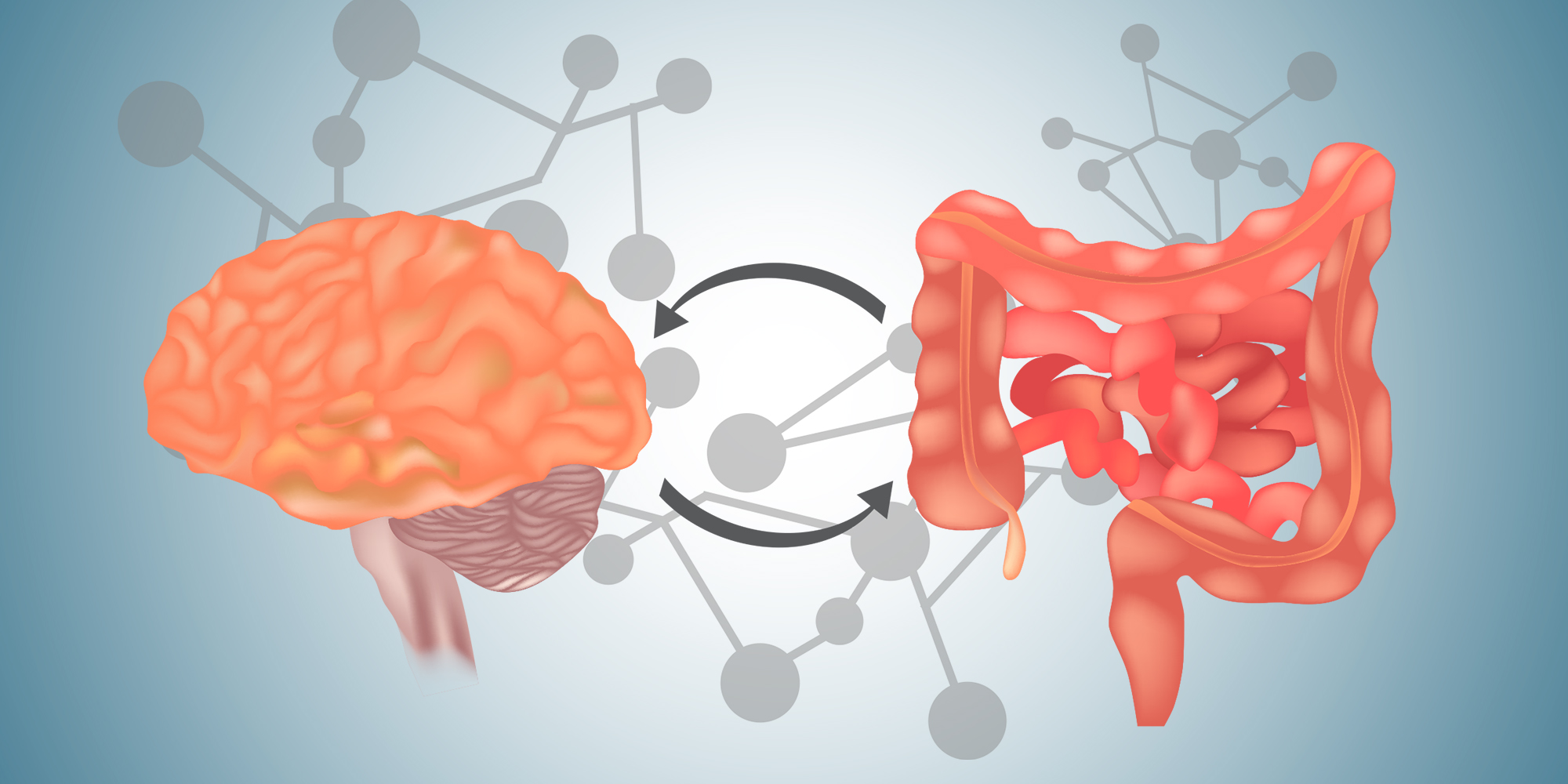
Categories: Digestive Health, Health & Wellness, Behavioral Health
 By Sarah Kinsinger, PhD, Digestive Health Program, Director of Gastrointestinal Behavioral Medicine Program
By Sarah Kinsinger, PhD, Digestive Health Program, Director of Gastrointestinal Behavioral Medicine Program
We all understand what it means to have a "gut feeling," or to feel a clenching in your gut when you realize you missed an important deadline.
But how is it that emotions can be experienced in your gut?
There have been many scientific advances in the past 10 years that have greatly improved our understanding of how the brain and the gut are connected and how we can improve gut health through mind-body medicine.
What is the brain-gut connection?
The digestive system has its own nervous system, called the enteric nervous system. It has over 100 million nerve endings and in many ways, it can control digestion independently without your conscious awareness.
The enteric nervous system has been nicknamed our "second brain.” This gut-brain is intimately connected to our "big brain" via a network of nerve pathways and the two nervous systems share many of the same neurotransmitters to facilitate communication.
In fact, 95% of serotonin is found in the gut! This bidirectional pathway is referred to as the brain-gut axis and involves moment-to-moment communication to control digestion.
This pathway explains why your stomach may start growling at the sight of a juicy steak, before the food even hits your stomach.
Can stress give me a stomach ache?
The brain-gut axis also explains how you can feel stress and emotions in the gut. Most people have experienced butterflies before a first date or diarrhea before public speaking.
These "gut feelings" are the result of stress being communicated to the gut via these bidirectional nerve pathways. For many patients, living with unpredictable GI symptoms can be highly stressful on its own.
Having to find a bathroom at a moment's notice or feeling uncomfortably bloated at a party can trigger stress and anxiety, which further aggravates the gut, creating a vicious cycle.
Can stress cause a gastrointestinal illness?
Individuals with a chronic digestive condition, such as irritable bowel syndrome (IBS) or inflammatory bowel disease (like Crohn's disease, ulcerative colitis) may be particularly sensitive to the effects of stress.
However, these are complex disorders and experts do not believe that stress causes these conditions. We do believe that stress can aggravate symptoms through brain-gut interactions, and patients are keenly aware of this association.
70% of patients with Crohn's disease and ulcerative colitis believe that flare-ups of their disease are related to stressful events. And researchers have confirmed a connection between stress and the gut. For example, animal studies have shown that stress can instigate inflammation in the colon or reactivate the disease when it has been in remission.
Therefore, stress can play an important role in the course of a digestive disease, even if it is not the initial cause.
What is a "sensitive gut"?
Some individuals are thought to be particularly sensitive to the effects of stress, and they are referred to as "gut responders." This gut sensitivity is thought to play an important role in functional gastrointestinal diseases, such as irritable bowel syndrome (IBS).
Experts refer to this as “visceral hypersensitivity,” meaning that the nerves of the gut are overly sensitive and firing in response to normal digestion. This is why for some individuals, a normal sized meal or the movement of gas through the intestines can cause severe pain, whereas for a healthy individual these sensations would be barely noticeable.
The brain also plays an important role and influences how these sensations in the gut are experienced. Brain imaging studies have shown that individuals with IBS have abnormalities in how their brains process signals from the gut, failing to properly tune out painful stimuli.
This breakdown in brain-gut communication is an important component for many digestive conditions and why we need to consider the role psychological factors when we treat patients.
How can I use my mind to heal my gut?
Medicine is moving towards a more holistic approach to treating patients, and there is growing interest in finding non-medication treatment options. GI diseases are a great example of the positive effects of mind-body interventions on health.
Because of the brain-gut axis, we can use psychological treatments to directly influence digestion. For example, hypnotherapy seems to have a quieting effect on the gut and has been shown to directly influence gut motility, gut secretions, and pain sensitivity.
Cognitive-behavioral therapy and gut-directed hypnotherapy are evidence-based treatments for IBS and have been shown to benefit patients' symptoms. Gut-directed hypnotherapy has even been shown to prolong remission in patients with ulcerative colitis.
Through these treatment approaches, patients can learn to regulate their stress response and reprogram the brain to tune out unwanted pain signals from the gut.
Sarah Kinsinger, PhD, practices behavioral gastroenterology and is the director of the gastrointestinal behavioral medicine program in the digestive health program at Loyola Medicine. Her clinical interests include cognitive behavioral therapy, inflammatory bowel disease (IBD), irritable bowel syndrome and medical hypnosis. She is also a board-certified health psychologist.
Dr. Kinsinger earned her doctorate in clinical psychology from the University of Miami and completed a residency in health psychology at the VA Puget Sound Health Care System and a fellowship in health psychology at the University of Illinois Medical Center at Chicago.
Book an appointment today to see Dr. Kinsinger by self-scheduling an in-person or virtual appointment using myLoyola.
