Understanding Spinal Stenosis: Symptoms, Causes, and Treatment Options
April 14, 2025
Categories: Spine
Tags: cervical spinal stenosis, lumbar spinal stenosis, spinal stenosis
Degenerative spinal changes affect up to 95% of people by age 50. Among these changes, spinal stenosis, a narrowing of the spaces within your spine, is a common condition that can significantly affect your quality of life. This condition typically affects the cervical (neck) and lumbar (lower back) regions of the spine by placing pressure on the spinal cord and nerve.
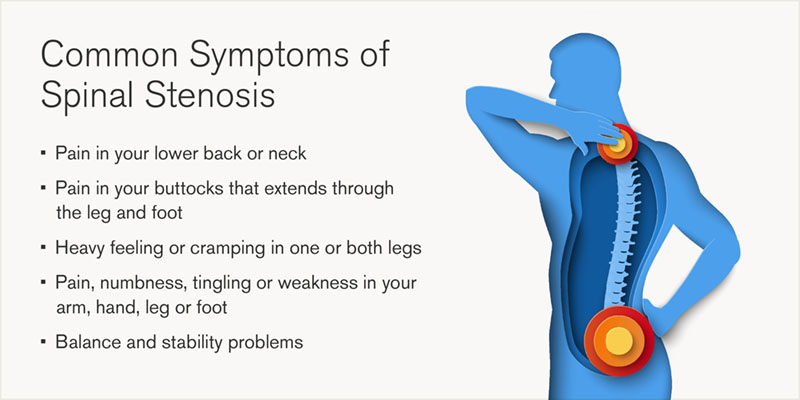
Symptoms of spinal stenosis
The symptoms of spinal stenosis vary depending on the location and severity of the narrowing. Common symptoms include pain, numbness, tingling, and muscle weakness. Patients may experience difficulty walking, balance issues, and, in severe cases, bowel or bladder dysfunction. These symptoms worsen over time, especially if the condition is left untreated.
Causes of spinal stenosis
Spinal stenosis is primarily caused by age-related degenerative changes in the spine, which gradually lead to a narrowing of the spinal canal. Several structural changes contribute to this condition:
Ligament changes
Over time, the ligaments that support the spine — particularly the ligamentum flavum — can become thicker and stiffer due to chronic inflammation and wear. These ligaments may also calcify, meaning they develop bony deposits that further encroach on the spinal canal, reducing space for the spinal cord and nerves. Thickened ligaments can lead to compression, worsening symptoms such as pain, numbness, and weakness in the extremities.
Intervertebral disc degeneration and bulging discs
The intervertebral discs, which serve as cushions between the vertebrae, naturally lose water content and elasticity with age. This degeneration causes them to lose height and become less effective at absorbing shock. In some cases, the weakened outer layer of a disc can bulge outward (known as a bulging disc) into the spinal canal, adding to the narrowing and contributing to nerve compression. If the disc bulges significantly or herniates, it can press directly on the spinal cord or nerve roots, leading to pain and neurological symptoms.
Bone spurs (Osteophytes)
The vertebrae respond to ongoing stress and degeneration by forming bony outgrowths called osteophytes, commonly known as bone spurs. These spurs develop along the edges of the vertebrae and facet joints as a result of osteoarthritis and the body’s attempt to stabilize the spine. However, rather than helping, bone spurs can protrude into the spinal canal or narrow the foramina (openings where nerves exit the spine), leading to nerve compression, inflammation, and increased pain or weakness in the arms and legs.
These degenerative changes, often occurring together, reduce the available space in the spinal canal, leading to pressure on the spinal cord and nerves, which characterizes spinal stenosis. Symptoms may range from mild discomfort to severe pain, tingling, and difficulty walking or maintaining balance.
Diagnosis and treatment options for spinal stenosis
Diagnosing spinal stenosis involves a thorough medical history and physical examination. Imaging studies such as x-rays, MRI, and CT scans are important as they can help identify the specific areas of compression and guide the treatment plan.
Treatment for spinal stenosis can be either non-surgical or surgical, depending on the severity of the symptoms and the degree of spinal canal narrowing.
- Physical therapy: Tailored exercises can help strengthen the muscles around the spine, improve flexibility, and reduce pain.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and pain relievers can manage pain and inflammation.
- Epidural steroid injections: These can reduce inflammation and provide temporary pain relief.
- Lifestyle modifications: Weight management, avoiding activities that worsen symptoms, and using supportive devices can help manage the condition.
When non-surgical treatments fail to alleviate symptoms, or if neurological deficiencies develop, surgical intervention may be necessary. Common surgical procedures include:
- Laminectomy: Surgery to remove part or all of the lamina (back part of a vertebra) to relieve spinal cord or nerve pressure.
- Foraminotomy: Expands the neural foramen (nerve exit openings) by removing bone or tissue to ease nerve compression.
- Spinal fusion: Permanently joins two or more vertebrae using bone grafts and hardware to stabilize the spine.
Finding relief from degenerative spinal changes
Early diagnosis and appropriate management of age-related degenerative spinal changes are crucial steps to prevent worsening symptoms and improve patient outcomes. Many individuals with spinal stenosis can find relief and remain active through a combination of lifestyle changes, physical therapy, medications, and surgery if needed.
Paul Arnold, MD, is a Neurosurgeon at Loyola Medicine specializing in treating patients with disorders of the lumbar cervical spine area. He treats mainly degenerative issues but also sees patients with fractures, trauma, infections, and tumors on the spine. He earned his medical degree from the University of Illinois at Chicago College of Medicine where he also completed his residency.
Visit loyolamedicine.org/spine to learn more.
