Understanding and Overcoming Menopause-Related Musculoskeletal Pain
March 14, 2024
Categories: Women's Health, Sports Medicine, Orthopaedics
Tags: menopause
 By Eliza J. Pierko, MD, Orthopaedic Sports Medicine
By Eliza J. Pierko, MD, Orthopaedic Sports Medicine
Menopause is a significant phase in a woman's life. It marks the end of her menstrual cycle and comes with many physical and emotional changes. Among these changes, musculoskeletal pain — discomfort in muscles, bones, and joints — is a common yet often overlooked symptom. Whether you're navigating this transition yourself or supporting someone who is, understanding and overcoming menopause-related pain is crucial for improving the quality of life.
Eliza J. Pierko, MD, a sports medicine physician at Loyola Medicine, spoke about the connection between menopause and musculoskeletal pain and how women can find relief.
"While the years approaching menopause can be frustrating, both mentally and physically, for many women, it is possible to find relief by coordinating with your health care provider and learning more about this time in every woman's life," says Dr. Pierko.
What is the connection between menopause and musculoskeletal pain?
Musculoskeletal pain affects the body's muscles, ligaments, tendons, and bones. The pain can range from short-lived discomfort to chronic pain that persists over months or even years. Many women will experience joint stiffness, muscle aches, or bone pain during perimenopause.
Causes of musculoskeletal pain vary and can include aging, physical strain, injuries, and autoimmune diseases. In the context of menopause, hormonal changes play a pivotal role in the onset and intensity of these symptoms.
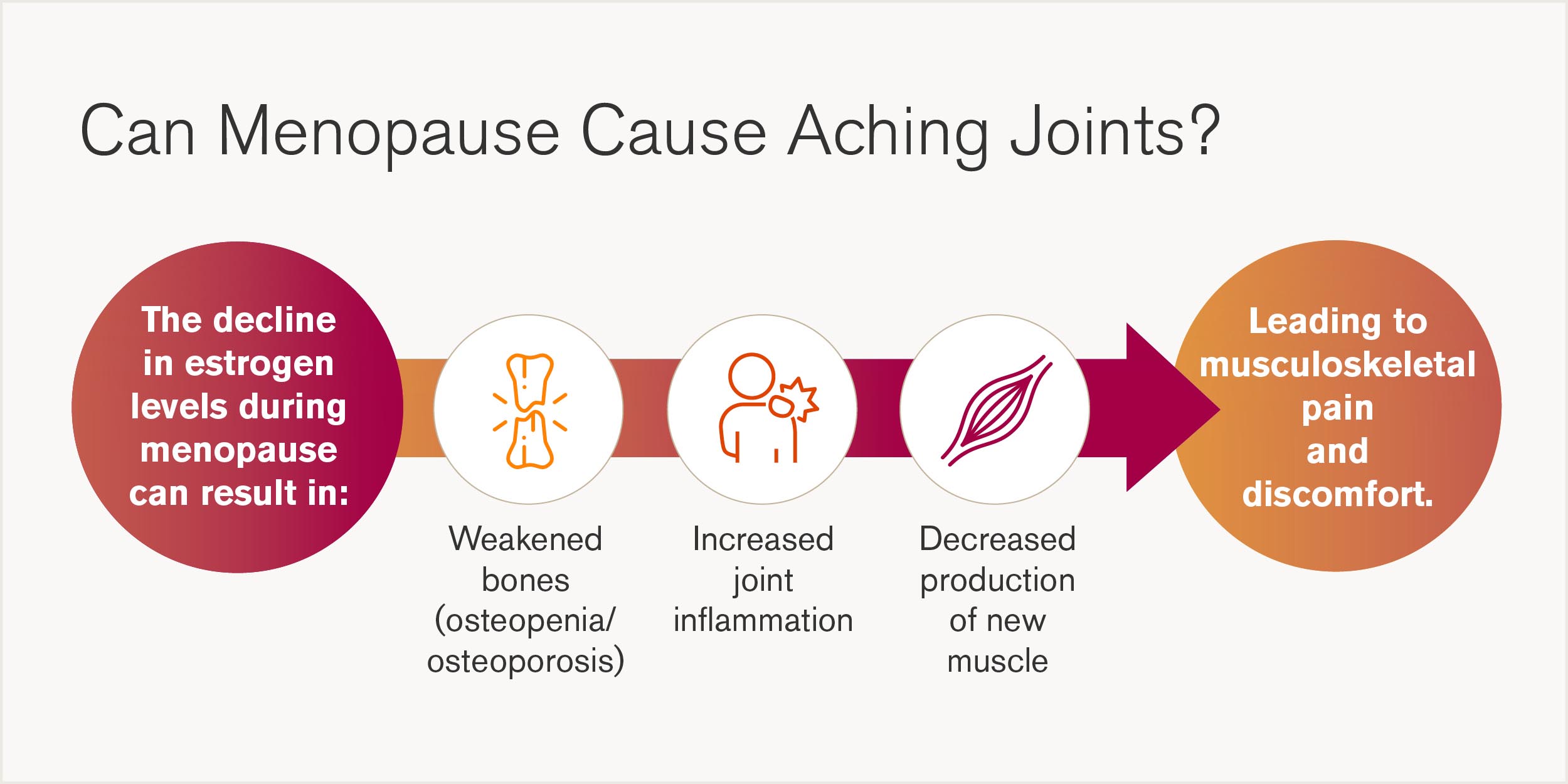
The connection between menopause and musculoskeletal pain revolves around hormonal fluctuations. Estrogen is the sex hormone responsible for the development and regulation of the female reproductive system and secondary sex characteristics. It also helps regulate the maintenance of bone, muscle health, and control of inflammation.
As estrogen levels drop during perimenopause, women may experience discomfort. This decline can lead to weakened bones, also known as osteopenia and osteoporosis, and contribute to joint and muscle pain development. Additionally, a decrease in muscle stem cells prevents the production of new muscle.
"How quickly estrogen levels start to decline is based on the individual woman. During the perimenopause period, levels fluctuate and become unpredictable. Eventually, production falls to a very low level," says Dr. Pierko.
"This means that you can have one symptom one day and an entirely different symptom the next. The intensity of symptoms can also fluctuate in the years leading up to menopause."
Because of the fluctuation in hormones during perimenopause, research indicates that women are at a higher risk for osteoarthritis, a type of joint disease that results from bone and cartilage wear and tear, low bone mineral density and loss of muscle mass.
How to treat menopause-related musculoskeletal pain
From medical treatments to lifestyle changes, women have many options when it comes to treating pain during menopause. However, while some treatments can be done at home, speaking with a health care professionals is important. They can provide options based on your individual symptoms and pain levels, helping speed up treatment and get you closer to being pain-free. There are many treatments your physician may suggest.
Lifestyle modifications
Diet: Nutrition plays a crucial role in bone and muscle health. Prioritize adequate amount of high quality protein to maintain lean muscle mass. Incorporate foods rich in calcium and vitamin D, such as leafy greens, beans, legumes, mushrooms, dairy products, and fortified foods, along with regular sunlight exposure. The anti-inflammatory Omega-3 fatty acids in chia seeds, flaxseeds and fish are also beneficial.
Exercise: Regular physical activity is key to managing musculoskeletal pain. Weight-bearing exercises, like walking, running, hiking, rope jumping strengthen bones and muscles, while yoga can improve flexibility. Follow the general guidelines of 150 minutes of moderate-intensity aerobic activity per week.
"Exercise, especially strength training, is extremely important for everyone, especially women. Women, on average, can lose 10 to 20% of lean body mass during perimenopause. I recommend at least two to three sessions per week of heavy lifting to combat this. If you've never done strength training, start with body weight exercises then work up to lifting heavier weights," says Dr. Pierko.
Medical treatments
Hormone replacement therapy (HRT): For some women, HRT can alleviate menopausal symptoms, including musculoskeletal pain, by replenishing estrogen levels. However, discussing the benefits and risks with a health care provider is important
"I highly recommend that women at least consider HRT. Muscle aches and pains improve in many patients when they begin this therapy. However, if a patient has a prior history of pulmonary embolism or blood clots in the legs, as well as personal or family history of breast cancer, it will require further discussion about risks and benefits with a specialist," says Dr. Pierko.
Other therapies: Treatments such as physical therapy and acupuncture can offer relief from pain. Acupuncture may reduce muscle pain by targeting specific tender points in the body, while physical therapy can help improve mobility and strength.
Home remedies
Heat and cold therapy: Applying heat pads can soothe stiff joints and muscles, while cold packs can reduce inflammation and swelling. Alternating between the two can be particularly effective for some women.
Over-the-counter pain relief: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can provide temporary relief. Supplements such as glucosamine and chondroitin may also offer benefits, though it's best to consult with a health care provider before starting any new supplement.
When should you seek professional help for menopause-related musculoskeletal pain?
While lifestyle changes and home remedies can significantly improve musculoskeletal pain, you should recognize when professional medical advice is needed. If you experience severe or persistent pain that interferes with daily life, signs of osteoporosis (like a sudden backache or height loss), or if your symptoms don't improve with self-care, it's time to seek help.
Is menopause-related pain keeping you from enjoying athletic and fitness activities? The women's sports medicine team works with you through your entire athletic journey to understand, prevent and treat your unique needs, so you can get back to the activities you love.
Eliza J. Pierko, MD, is a sports medicine specialist at Loyola Medicine. Dr. Pierko completed her residency at Presence Saint Joseph Hospital and fellowship at MacNeal Hospital. She has been helping runners overcome their injuries since then. She herself is a marathoner, triathlete and belongs to a women physicians running group. Her clinical interests include providing comprehensive care for active women.
Book an appointment today to see Dr. Pierko by self-scheduling an in-person or virtual appointment using myLoyola.
How to Schedule a Loyola Appointment
You can easily self-schedule an appointment online today with one of Loyola Medicine's expert primary and specialty care providers!
Join our Mailing List
Stay up to date with the latest news, health tips and more from Loyola Medicine!
