What to Expect If You Need a Bone Marrow Transplant
February 1, 2024
Categories: Transplant, Cancer Care
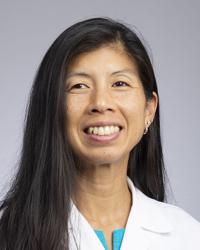 By Stephanie Tsai, MD, Hematology & Oncology
By Stephanie Tsai, MD, Hematology & Oncology
Needing a bone marrow transplant can be scary. Your bone marrow is the foundation of your immune system. If a transplant is needed, it means that one has a serious condition, such as leukemia, lymphoma, and immune deficiency disorders.
We spoke with Stephanie Tsai, MD, the Unit Medical Director of the Division of Hematology/Oncology at Loyola Medicine, to learn about what patients can expect if they need a bone marrow transplant.
"A bone marrow transplant can be recommended for a number of reasons. It is often complex so it's good to speak with a provider and follow their recommendation for the best chance at long-term health," says Dr. Tsai.
What are the different types of bone marrow transplants?
There are two main types of bone marrow transplants. The main difference between the two is where the stem cells being used are taken from.
Autologous transplant
An autologous bone marrow transplant involves using the patient's own stem cells. Stem cells are collected from the patient before the process begins. This type is typically recommended for patients with certain types of cancers, such as lymphomas or multiple myeloma. The collected stem cells act as a form of "self-rescue" after high-dose chemotherapy.
Allogenic transplant
An allogeneic bone marrow transplant involves using stem cells from a donor, sometimes a matched sibling (only 20-30% have a matched sibling) or often an unrelated donor can be used. The donor's cells provide the patient with a new immune system to help eliminate cancer cells in the patient more permanently. Recommended for patients with certain types of leukemia, severe aplastic anemia, or genetic disorders, it typically requires a suitable donor with a closely matched tissue type.
How to prepare for a bone marrow transplant
If you and your doctor decide a bone marrow transplant is the right choice for you, they will guide you through the process. Typically, your doctor(s) will discuss your options and work with you on:
- Health assessment: A comprehensive evaluation of your health will be conducted at the hospital or cancer center. This includes a detailed medical history and a physical examination.
- Donor search: If you require an allogenic transplant, your team will collaborate with you to identify the most suitable donor.
- Financial considerations: You have the opportunity to consult with a financial counselor who will address the expenses associated with the treatment.
- Preservation of fertility: The intensive chemotherapy and radiation administered before a bone marrow transplant can impact fertility. Some individuals wish to preserve the possibility of having biological children.
- Conditioning: Approximately 5 to 10 days prior to your procedure, you will be admitted to the hospital or outpatient clinic. During this period, you will undergo a conditioning regimen to prepare your body. Multiple doses of chemotherapy, full-body radiation, or a combination of both will be administered to weaken or eliminate cancer cells and unhealthy bone marrow, as well as to suppress your immune system so that you may accept the donor's cells.
Before a bone marrow transplant, your doctor will provide guidelines to optimize your health and well-being to have the best chance at a successful procedure. These lifestyle changes may include:
- Diet: Getting enough calories and nutrients each day will be important for keeping your strength up throughout the process.
- Exercise: A strong body responds better and recovers faster.
- Designate a caregiver: Your full attention and energy should be focused on your recovery. Having a family member or friend help you during this time is critical.
- Living arrangements: Whether you have a transplant as an inpatient or outpatient, you will want to think ahead to where you will stay during recovery. Your immune system will be compromised after the procedure so a clean environment that is not far from the cancer center is essential.
What happens during a bone marrow transplant?
Despite the extensive preparation, the entire transplant process is actually relatively simple and straightforward. It is a painless procedure where you are entirely awake, not under any anesthesia. The process typically takes less than one to two hours during which stem cells are infused into your body through a central line. If you have a donor, healthy cells will usually be collected through an IV catheter (similar to donating blood) and transfused into you.
Through a process called engraftment, the healthy cells will travel to your bone marrow and multiply, creating new healthy cells. It usually take multiple weeks before your body returns to the standard blood cell range.
How to recover from a bone marrow transplant
Recovery following a bone marrow transplant is a crucial phase where the patient's body begins to heal and adapt to the new cells. During the initial recovery period, patients are monitored closely to detect and manage any potential complications. This includes monitoring for signs of infection, graft-versus-host disease (GVHD), and other post-transplant issues.
Patients will receive supportive care, such as medications to prevent infections, support ongoing engraftment/prevent rejection, pain management (if needed), and other measures to address specific needs.
Patients will observe the gradual recovery of white blood cells, red blood cells, and platelets. This recovery is a positive sign that the transplanted cells are functioning effectively. However, as the new immune system develops, patients remain more susceptible to infections for a longer period of time. Precautions and medications are employed to manage and prevent infections during this vulnerable period.
"Patients will usually stay in the hospital for a couple of weeks to be monitored and make sure there is an acceptable risk of infection due to their new developing immune system, and that they are adequately functional. However, afterwards, many patients want to go home. At that time, we provide guidelines for caretakers to follow with close follow-ups in the cancer center," says Dr. Tsai.
In the long-term, patients will have regular follow-up appointments to monitor their overall health, blood counts, and any potential long-term effects. After a period of recovery, patients will need to catch up on vaccinations to protect against preventable diseases.
Stephanie Tsai, MD, is the Unit Medical Director of the Division of Hematology/Oncology at Loyola Medicine and the leader of the Loyola Leukemia Research Program. She specializes in treating hematology disorders and cell therapies such as bone marrow transplant. During appointments, she emphasizes comprehensive and compassionate care to patients while applying the latest advances, therapies, and available knowledge.
Dr. Tsai earned her medical degree from the Boston University School of Medicine and completed a residency in internal medicine at Boston Medical Center.
