Training, Clinical Rotations & Program Education
Clinical Rotations and Education Experience
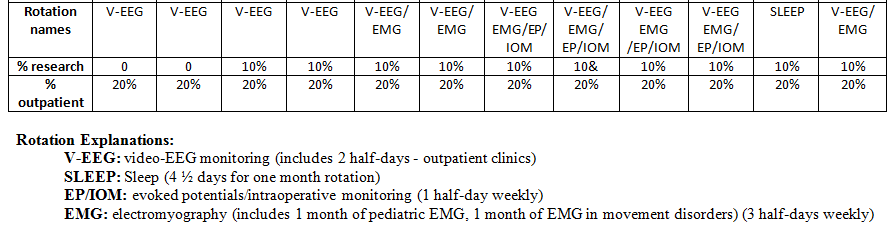
Electroencephalography (EEG) Rotation
The electroencephalography (EEG) laboratories perform inpatient and outpatient EEG’s, bedside recordings when needed, intensive care monitoring and EEG studies for suspected cerebral death. Fellows will gain competence in these studies. This could include weekly participation in an epilepsy clinic.
As part of the fellowship program, patients need to be admitted to the hospital for epilepsy monitoring. This is to clarify and evaluate patients' seizures with EEG and video monitoring. Fellows read EEG’s on a regular basis with attending neurophysiologists and are involved in all aspects of LTME.
LTME is the synchronized recording of behavior and EEG for prolonged periods ranging from a few hours to over one week. The objectives of monitoring patients in this manner are any one of the following:
- Establish a diagnosis of epilepsy.
- To clarify the nature of events that patients suffer. Synchronized video telemetry is necessary to analyze behavior with the EEG activity.
- To track the course of some cases of status epilepticus.
The goals for EEG rotation are:
- Mastering the practical aspects of EEG recording techniques using the 10-20 International System. This includes use of different montages and the effects of changes in filters as well recording sensitivity. The residents will learn to recognize artifacts and how to correct them.
- To understand relevant basic electronics including polarities, resistors, capacitors and amplifiers.
- Recognize EEG patterns of normal and abnormal brain electrical activity.
- Interpret the EEG findings in a meaningful fashion in their clinical context.
- Understanding and interpretation of LTME as well as its clinical usefulness.
This includes following patients in the hospital with daily review of EEG and video recordings with the attending neurophysiologists. Weekly conferences to discuss interesting cases and/or cases being evaluated for epilepsy surgery are conducted.
EEG and video monitoring readily allows for the capture of epileptic events. The fellow can then study the electroencephalogram evolution of a seizure in real time.
Electromyography (EMG) Rotation
Gradually increasing levels of responsibility, didactic sessions, guided reading, and videotapes are used to teach the clinical neurophysiology fellows. The fellows are expected to gain competence in the following areas:
- Basic electronics
- Motor conduction studies
- Sensory conduction studies
- H reflexes and F-waves
- Needle electromyography
- Autonomic studies (sympathetic skin responses, R-R interval variation)
The fellows will be expected to perform the studies independently requiring knowledge of electrode application, stimulus sites and intensities, needle electrode placement, and equipment use. The fellows will be exposed to single fiber EMG studies.
The fellows will be expected to understand the physiology of these studies, the relevant anatomy for performing the studies, normal findings and the interpretation of abnormal studies.
Based on clinical information and their knowledge of EMG procedures, they will be expected to design examinations that can produce meaningful clinical information.
Evoked Potentials Rotation
The fellows will learn evoked potentials by observation, performing the studies, and guided reading. The fellows will be expected to have competency in the following areas:
- Somatosensory evoked potentials
- Visual evoked potentials
- Brainstem evoked potentials
For each of the evoked potential studies, the fellows will be expected to know how to perform these studies including electrode application, stimulation, and equipment use.
The fellows will be expected to understand the physiology of the evoked potentials, normal and abnormal values, the anatomical localization of abnormalities, and the relevance of these abnormalities for clinical diagnosis.
Sleep Medicine Rotation
The diagnostic sleep laboratories provide a high level of expertise in the performance and interpretation of sleep disorders by board certified practitioners. The practical training in clinical sleep medicine to residents is part of a comprehensive, interdisciplinary sleep medicine training program with two sleep laboratory sites and close affiliation with the division of pulmonary and critical care medicine of the department of medicine.
Multichannel attended nocturnal polysomnograms are performed. The parameters measured include EEG, electrooculography (EOG), chin EMG, leg EMG, ECG, nasal air flow, oral air flow, Respitrace, oxygen saturation, snoring, videotaping and sleep stage scoring.
Split night studies are performed if the patients meet the criteria for this as established by practice parameters of the American Academy of Sleep Medicine.
The goals for the sleep medicine rotation are:
- To provide practical training in clinical sleep medicine during sleep clinic and sleep laboratory rotations.
- Competence in the interpretation of the sleep disorders from the sleep records.
- Broad expertise in clinical sleep medicine, development of research interests, and preparation for board certification in sleep medicine. The training should also allow the residents to develop and improve sleep health care in their practices or institutions.
Research Rotation
The fellows will be expected to complete one research project in clinical neurophysiology. These projects will be mentored by one of the clinical neurophysiology faculty. It is expected that they will result in work suitable for publication in peer-reviewed journals.
From these projects, the fellows should attain experience with research techniques in clinical neurophysiology. The experience should also enable the residents to better evaluate the clinical neurophysiology literature.
