Clinical Rotations & Training
Clinical Rotations
"4+2" System
Rotations are scheduled into cyclic six-week chunks, four weeks of which are spent on a service. One of the remaining two weeks is a week dedicated to the outpatient experience (continuity clinic and elective subspecialty clinics). The final week becomes either vacation, night float week at Loyola, or an elective week.
This system has afforded several advantages: It has helped provide a more consistent inpatient and elective experience, allows for more dedicated time in the continuity clinic (weeks aren't interrupted by continuity clinic time), helps residents to remain "fresh" by avoiding uninterupted months-after-months of inpatient service, and allows one to experience a broader range of Neurology in the PGY2 year.
PGY2 year is spent mostly on inpatient services at Loyola or at Hines VA. PGY3 and PGY4 years come with increased autonomy, increased elective time, more leadership opportunities, and relatively less call.
Two Clinical Rotation Sites

Loyola University Medical Center has 547 beds, over 20,000 admissions annually, and nearly 50,000 emergency department visits annually.
Hines Veterans Hospital is among the largest veterans medical centers in the nation, with 485 beds and an expansive campus. It has nearly 10,000 admissions annually and over 25,000 emergency department visits annually.
The two large campuses are adjacent to one another. In the above photo, the Loyola campus can be seen in the foreground and the Hines VA campus in the background. All areas are within walking distance of each other.
Our Services Managed by Our Residents
- Loyola Stroke (Vascular) Service
- Loyola General Neurology Service
- Loyola Neuro-ICU Service
- Loyola Pediatric Neurology Service
- Loyola EEG/EMG Service
- Hines VAH Neurology Inpatient Service
- Hines VAH Neurology Consultation Service
Continuity Clinic
The "4+2" scheduling system allows us to dedicate every sixth week to the outpatient setting. Every PGY2-PGY4 resident has his or her own continuity clinic at both Loyola and Hines VA. There are several half-days during clinic week that are spent in elective subspecialty clinics and at "Friday school."
Elective Opportunities
Elective rotations include: Cerebrovascular Disease, Endovascular Neurology, Neuromuscular/EMG, Epilepsy/EEG, Headache, Multiple Sclerosis, Sleep Medicine, Neurocritical Care, Neuro-Ophthalmology, Neurosurgery for the Neurologist, Movement Disorders, Neuropsychiatry, Neuropathology and Neuroradiology.
On Call
We use a night float system at Loyola - a resident covers the hospital from 5pm-6am in weeklong chunks (with Friday nights off). There is typically no call during a resident's clinic week. We strictly adhere to duty hour restrictions. All PGY2-PGY4 residents take their share of call, though the system is graduated so that more-senior residents take relatively less.
Sample Resident Schedule
Resident Education
Dr. José Biller
Dr. Biller is the Chairman of the Department of Neurology and plays an integral role in the training of Loyola Neurology residents. We challenge our applicants to find another residency program in which the department chairperson is so deeply involved with day-to-day resident education and workflow. He is an author of of several widely read and comprehensive textbooks such as Practical Neurology, Localization in Clinical Neurology, Concise Neurology, The Neurologic Examination, and most recently, The Hospital Neurology Book. He has lectures and didactic sessions with the residents at least once per week and shapes much of our curriculum.
Dr. Biller is an internationally renowned academician. He has published more than 310 peer-reviewed articles, more than 130 book chapters, edited 25 books, and given more than 600 lectures around the world. He served as director of the American Board of Psychiatry and Neurology (ABPN) from 1994 to 2001 and as president of the ABPN in 2001. He is the editor of the Journal of Stroke and Cerebrovascular Diseases and Chief-Editor of Frontiers in Neurology, as well as being an editorial board member and reviewer for multiple other national and international journals and publications. The training the next generation of neurologists remains amongst his top priorities and greatest passions.
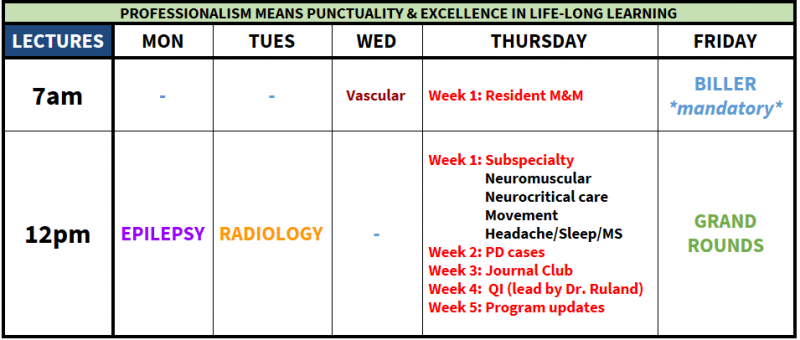
Conferences and Didactic Learning
Curriculum
With the "4+2" system dividing the year into about nine blocks (six weeks per block), it seemed natural to divide the curriculum into nine major groupings and focus on one per block. Examples include: vascular neurology, neuromuscular, epilepsy, headache, etc. Within that block, Friday school sessions are dedicated to that block's subject material and there are didactic lectures by corresponding subspecialists.
Friday School
On Friday mornings, during the "+2" weeks, small groups of residents get together to present topics to each other, go over cases, and go through practice board questions. Subject material is chosen based on the current academic block the residents are in. Various afternoons are "protected time" for studying, catching up on documentation, working on their CV or fellowship applications, etc. Residents appreciate these days because they are relatively low key and a nice change of pace.
Stritch School of Medicine
We are fortunate to work closely with Loyola University Chicago's very talented and driven medical students. At Loyola, neurology is a required rotation and lasts a month. Thus, we spend large amounts of time with medical students and have the privilige of assisting in their education during their clinical years. Our residents lead formal and informal medical student lectures and also lead lumbar puncture workshops for them in the medical school's simulation center.
Neuroscience Immersion Curriculum
Every June, as our interns wrap up their PGY-1 year and transition from the Department of Medicine to the Department of Neurology, the residents and faculty work together to provide a month of orientation, lectures, simulators and guided study that we deem our "Neuroscience Immersion Month." The "Stroke Code" simulator that was developed to train our new residents has been improved upon every year, winning an AAN QI award in 2015. The "Brain Death with Family Discussion Component" simulator has expanded each year as well, recently winning an AAN QI award in 2017. A "Status Epilepticus" simulator prepares you to face this neurologic emergency with confidence, as the "Lumbar Puncture" simulator prepares you for this common bedside procedure. The month leaves plenty of time for independent study as well. We try to make sure our newbies are as prepared as possible for July 1st of PGY-2 year.
Procedural Skills
Develop skills via workshops and advanced simulation sessions – lumbar puncture, botox injection for spasticity and headache, central line placement, status epilepticus, acute stroke, brain death and breaking bad news to families.
Practice those same skills on your rotations, as well as additional opportunities to participate in cerebral catheter angiography, emergent cerebral thrombectomy, stenting, aneurysm coiling, and more.
Scholarly Activity
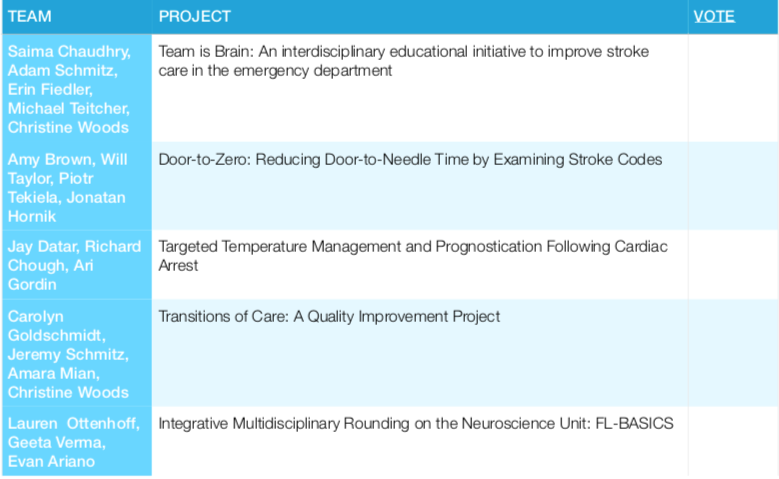
Brumlik Resident Research Symposium
Every academic year culminates in the Brumlik Symposium, held during the day of our evening graduation ceremony. The symposium is named after Dr. Joel Brumlik, MD, the first Chairman of Neurology at the Stritch School of Medicine at Loyola. Groups of residents present quality improvement projects that they have worked on throughout the academic year. The goal of the symposium is to provide a "built in" research experience during residency and also to have real and palpable impact on the culture and policies of the hospital they work in. Projects in the past have focused on medical education, transitions in care, patient safety, medication reconciliation, clinical efficiency and patient satisfaction. In addition to a "local" impact, the target for all projects is publication in peer-reviewed journals, presentation at national level meetings, and submission for the AAN Safety and Quality Award presented at the National Meeting.
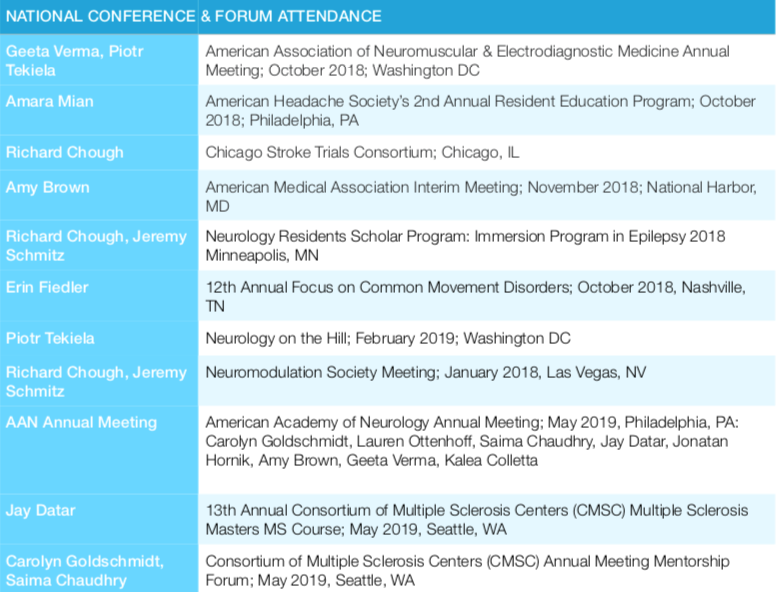
National Conferences and Professional Meetings
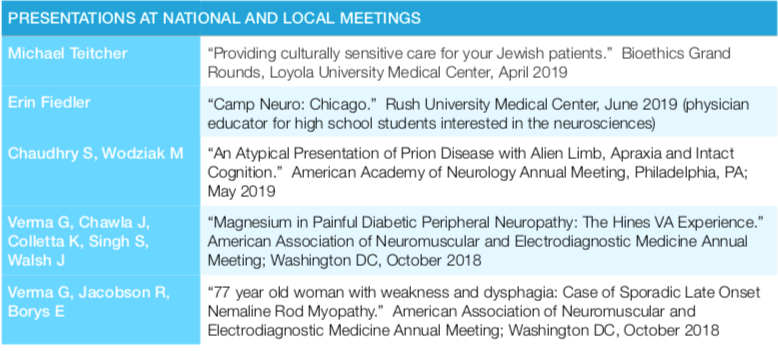
National, regional, and local academic conference attendance is encouraged and residents often present posters at national meetings. Residents receive an annual stipend that accumulates for the purpose of financial assistance when attending conferences.
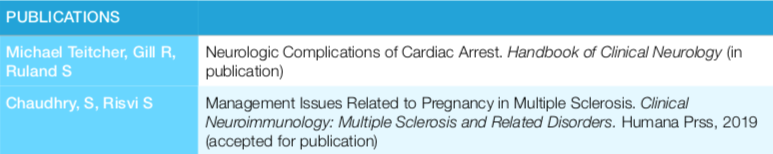
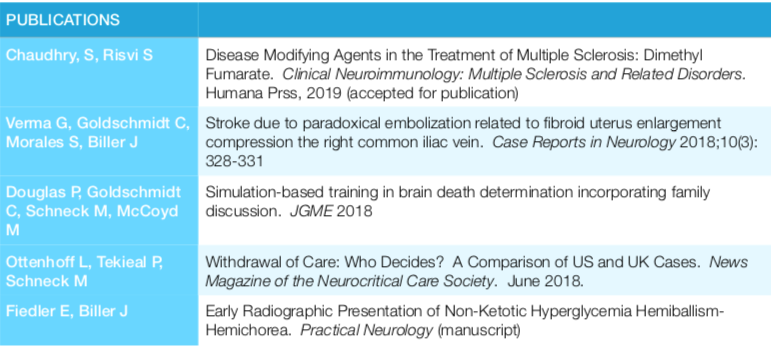
Recent Resident Publications
Recent Brumlik Symposium Presentations
Recent National Conference and Forum Attendance
Recent Presentations at National and Local Meetings
![]()
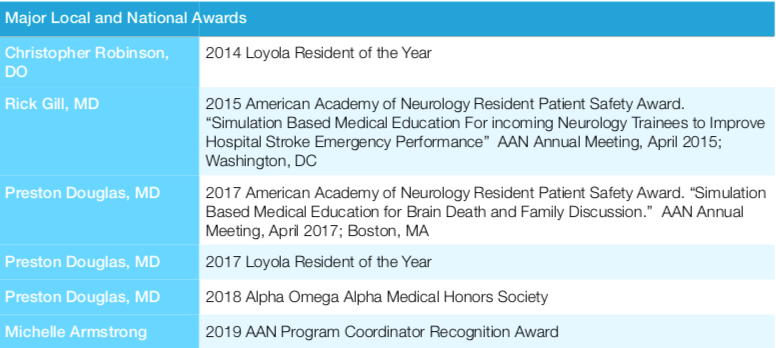
Recent Awards and Recognitions (Local and National)
Dr. Adam Wadina (Neurology PGY 3), was nominated by the SSOM as Resident Of The Year 2022.
Publications and Awards
Sergej Stjepic OMS-II, Bradley Boget OMS-II, Dr. David Dufeau PhD, Dr. Garren Gebhardt DO, (2018). Aesculapius: Adding a Dimension of Instruction Through Integrating Spatial Knowledge.
- Award: 3rd place award winning poster in Education
- Competition: LBORC/ AAO Research Convocation (Louisa Burns Osteopathic Research Committee/ American Academy of Osteopathy
- Date: April 2019
- Link: http://www.academyofosteopathy.org/2019-research-poster-winners
A publication
- Publication: Indiana Academy of Sciences (IAC)
- Conference: IAC 135th Annual Meeting
- Presentation: Abstract accepted for “Hot Topic” (30-60 minute lecture)
- Date: March, 2020
- Link: (2nd author at the beginning of page 23)
- https://www.indianaacademyofscience.org/MediaLibraries/IAS2018/Documents/135th%20Annual%20Meeting/135th-Annual-Meeting-Abstracts.pdf
Siemionow M, Strojny MM, Kozlowska K, Brodowska S, Grau-Kazmierczak W, Cwykiel J. Application of Human Epineural Conduit Supported with Human Mesenchymal Stem Cells as a Novel Therapy for Enhancement of Nerve Gap Regeneration. Stem Cell Rev Rep. 2022 Feb;18(2):642-659. doi: 10.1007/s12015-021-10301-z. Epub 2021 Nov 17. PMID: 34787795; PMCID: PMC8930890.
Siemionow M, Brodowska S, Langa P, Zalants K, Kozlowska K, Grau-Kazmierczak W, Heydemann A. Long-Term Biodistribution and Safety of Human Dystrophin Expressing Chimeric Cell Therapy After Systemic-Intraosseous Administration to Duchenne Muscular Dystrophy Model. Arch Immunol Ther Exp (Warsz). 2022 Aug 17;70(1):20. doi: 10.1007/s00005-022-00656-7. PMID: 35978142; PMCID: PMC9385806.
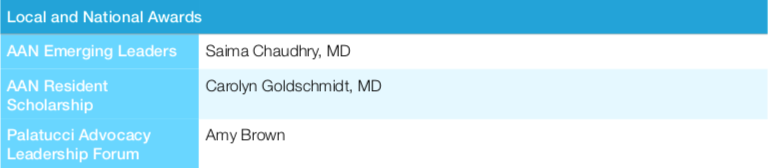
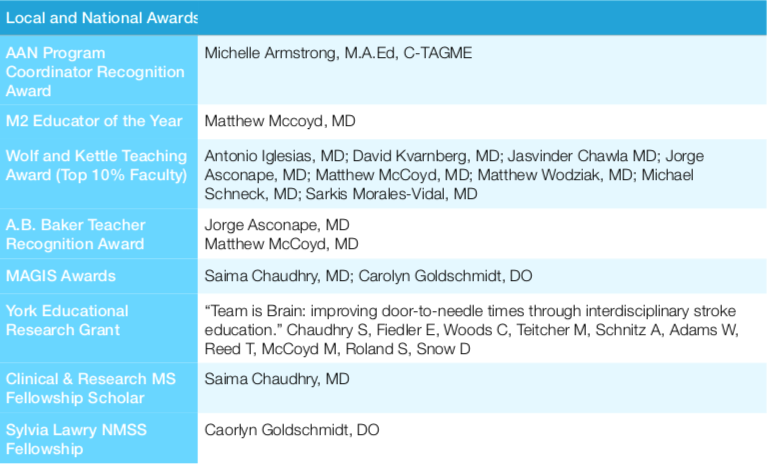
All-Time Major and National Awards (2014-2019)