Advanced Epilepsy Care: When Medication is Not Enough
January 31, 2022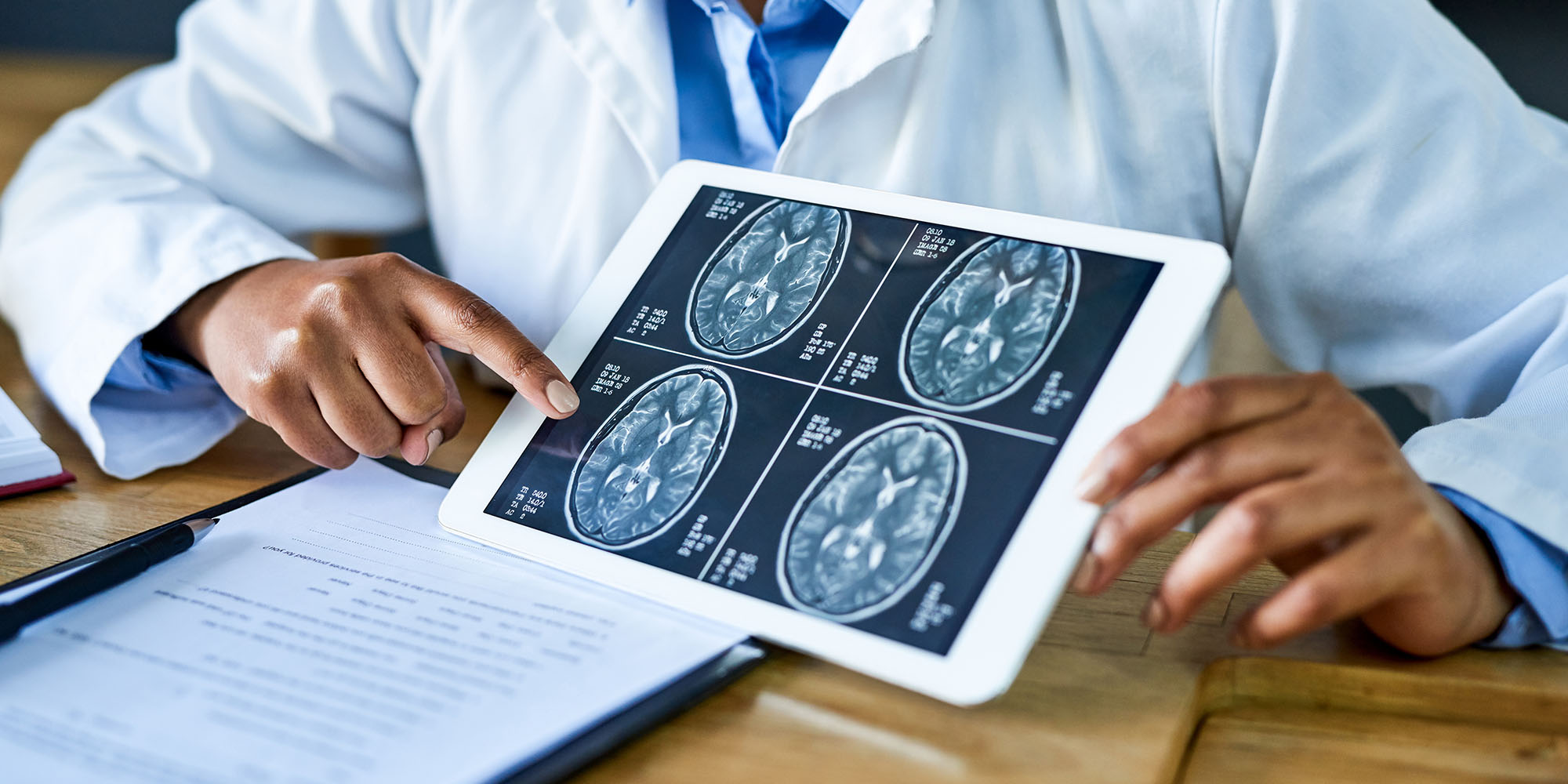
Categories: Neurology & Neurosurgery
Tags: Epilepsy
 By Jorge Asconapé, MD, Neurology
By Jorge Asconapé, MD, Neurology
Epilepsy is a condition of the brain that causes recurrent seizures. People with epilepsy and their families may experience stigma and a loss of control that can affect their quality of life.
Epilepsy can also be dangerous if a seizure occurs during activities such as driving, swimming or working.
The primary treatment for epilepsy is medication. For many people, medication is very effective at managing their symptoms.
Others discover their condition is resistant, or refractory, to medicine and require different treatment strategies.
Loyola Medicine epilepsy specialist, Jorge Asconapé, MD, answers questions to explain the treatment options available to patients with refractory epilepsy.
What causes epilepsy?
Seizures result from disorganized electrical activity in the brain’s networks of nerve cells.
Epilepsy can be caused by numerous conditions such as genetic disorders and damage from strokes, trauma or tumors.
What are the types of epileptic seizures?
We classify seizures two ways, generalized and focal:
Focal onset seizures
This seizure type affects two of three people with epilepsy. As many as 30% of them may not achieve complete seizure control on medication.
Focal seizures start in one location in the brain and may cause:
- Blank stares
- Confusion
- Convulsions
- Involuntary movements
- Strange sensations
Generalized onset seizures
About one in three people with epilepsy have generalized onset seizures. Genetic mutations present in every brain cell are usually the cause.
Generalized seizures can cause:
- Blank staring
- Convulsions
- Muscle twitches
How do surgeons treat refractory epilepsy?
Surgery may be a good option for people with focal onset seizures who do not respond to medications. Resective surgery consists of removing the area of the brain where seizures come from.
Relatively large areas of the brain may be removed with no negative neurological effects. About two thirds of patients that have this surgery become seizure free. Some are eventually able to stop medication.
We’ve been performing this surgery at Loyola for more than 20 years and have helped many patients become seizure-free.
How does stereo EEG help identify the location of the seizure?
Stereoelectroencephalography (stereo EEG or SEEG) is a diagnostic procedure where we insert multiple flexible electrodes into the brain.
When a seizure occurs, the electrodes detect the abnormal electrical activity of the brain. The result is a three-dimensional picture that shows us where the seizure starts. We use that information to plan surgery.
Previously, we inserted the electrodes manually with the use of a special frame, which was a long and tedious procedure for the patient.
Now, we use a sophisticated computer and MRI imaging to calculate each electrode’s path, and a robotic arm to insert the electrodes.
The benefits of stereo EEG include:
- Reduced surgery time from 12 to two hours
- Increased precision of electrode placement
- Increased safety since it decreases potential damage to blood vessels
- Less pain and faster healing because it requires small holes in the skull rather than the removal of a large area of skull
What are functional neurosurgical treatments for epilepsy?
Other options for treating epilepsy involve chronic electrical stimulation of the brain. They involve pacemaker-type devices and surgically implanted wires that deliver an electrical charge to a nerve or directly into the brain. Over time, they reduce the severity and frequency of seizures.
The Food and Drug Administration (FDA) has approved three functional neurosurgery treatments. They include:
- Deep brain stimulation: We place an electrode in the thalamus, a structure located in the center of the brain. A stimulator implanted under the skin sends out electrical signals at regular intervals to help control seizures.
- Responsive neurostimulation: With this device, we place the electrodes in the brain where the seizures start. A computer chip connected to the wires monitors your brain activity and detects the onset of a seizure. Within milliseconds, the wires deliver an electrical charge to disrupt the seizure.
- Vagus nerve stimulation: The vagus nerve is in your neck and transmits information between your brain and almost every organ in your body. We attach the wires to the nerve and implant the stimulator under your skin. The stimulator delivers electrical stimulation to the nerve at regular intervals to control seizure activity.
What is a level 4 epilepsy center?
We’re proud to be recognized by the National Association of Epilepsy Centers as a Level 4 Epilepsy Center, the highest level. We offer the most complex diagnostic monitoring and treatments available for epilepsy.
As a specialized Epilepsy Center, we also incorporate the essential elements of care, including:
- Interdisciplinary care teams that draw on specialists from across Loyola to support all aspects of your care
- Educational activities to provide continued educational opportunities for both patients and providers
- Quality-of-care performance measures that help us assess the care we provide and develop improvement strategies
- Safety protocols to reduce the risks from seizures while patients are in the hospital
When should patients seek specialized epilepsy care?
Patients with epilepsy should receive in-depth care. Epilepsy centers provide the latest diagnostic services and all types of advanced treatments.
This specialty care offers patients the most options when developing a treatment plan and a better chance of stopping their seizures.
In addition to being a Level 4 Epilepsy Center, we have epileptologists as part of our comprehensive care team. These neurologists have completed an epilepsy fellowship or are board certified in epilepsy. Our team also includes:
- Neuropsychologists who provide therapeutic care
- Neurosurgeons who perform the latest surgical techniques
To make an appointment today, call 888-584-7888 or schedule an appointment online.
Jorge Asconapé, MD is a neurologist at Loyola Medicine. He is board certified in neurology, clinical neurophysiology and epilepsy and specializes in treating epilepsy in adults and children. His research interests include improving care for patients with medication-resistant epilepsy and identifying new epilepsy treatments.
Dr. Asconapé received his medical degree from the University of Buenos Aires, Argentina. He completed his residency and fellowship at North Carolina Baptist Hospital of Wake Forest University.
Book an appointment today to see Dr. Asconapé or another Loyola specialist by self-scheduling an in-person or virtual appointment using myLoyola.
