Ventricular Assist Devices (VAD)
Overview and Facts about Ventricular Assist Devices (VAD)
What is a Ventricular Assist Device?
A ventricular assist device (VAD) is a surgically-implanted pump that helps the heart circulate blood to the rest of the body.
There are four types of VAD devices:
- Left ventricular assist device (LVAD) helps pump oxygen-rich blood from the left side of the heart out to the body. This is the most common type of VAD used.
- Right ventricular assist device (RVAD) helps pump oxygen-poor blood from the right side of the heart to your lungs.
- Biventricular ventricular assist device (BiVAD) helps pump blood from both left and right sides of the heart.
- Percutaneous (temporary) ventricular assist device (pVAD) helps pump blood from the heart out to the body. pVAD devices are not surgically implanted, but rather connected by inserting a tube into the femoral body (thigh bone) to the heart and leaving the pump outside of the body.
How Long Can a VAD Support My Heart?
Ventricular assist devices can support your heart in various ways, depending on your medical needs. Some devices are only used in the hospital to bridge the recovery from high-risk heart surgery, improve the patient's chances for a successful heart transplant, or transition to a durable implantable VAD. There are several FDA-approved short-term devices available at Loyola Medicine, allowing your medical care team to individualize your treatment plan by selecting the most beneficial device for you.
You may be given more long-term use devices. These are surgically implanted in the hospital to help patients with recovery and allow them to return home with the device in place. These may be used as a lead-in to transplantation or to recover from a recent injury to their heart.
Going home with a VAD allows patients to resume most of their daily activities, providing a familiar routine while they wait for a possible transplant. Patients who are not eligible for heart transplantation may be eligible for a long-term VAD device that would allow them to return home and minimize heart failure readmissions and improve their quality of life.
Evaluation for Advanced Heart Failure Therapies
Your cardiologist may recommend an evaluation of advanced therapy options for the treatment of your heart failure. Our advanced heart failure cardiology team will work with you to confirm your diagnosis of end-stage heart failure and start your VAD evaluation. The evaluation has several steps and we will guide you through the process.
Depending on your condition, the advanced heart failure cardiologist may request additional testing in addition to our routine evaluation to gain a comprehensive representation of your past and present health history.
Generally, the routine evaluation for VAD includes:
- Review of health history with the medical team
- Extensive cardiac testing
- Imaging
- Blood work
- Cancer screening
- Psycho-social consultation
- Palliative care consultation
There are barriers to VAD implantation, including alcohol and substance abuse problems, an inability to comply with treatment (such as following a complex medication plan), a lack of social and financial support, and uncontrolled or untreatable mental illnesses.
The Medical Review Board will discuss your case and decide whether a VAD would be a treatment option available for you.
What Can I Expect During a VAD Procedure?
VAD implantation is a major heart surgery that takes place in an operating room with a cardiothoracic surgeon specially trained to place these devices in patients. The surgery can take anywhere from four to six hours. Patient risks and recovery are determined individually and discussed with the patient at the time of evaluation.
Undergoing this surgery requires strong dedication from the patient, and the Loyola Medicine VAD team is committed to supporting the patient and their care team every step of the way through the journey. 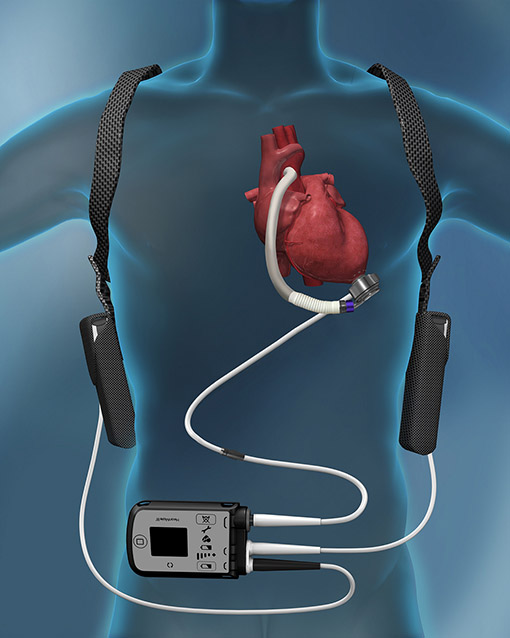
A VAD pump consists of four main parts:
- VAD pump: A mechanical pump surgically attached to the heart that works to help the weakened heart.
- Driveline: A tube connecting the pump inside the body to the controller outside the body. This tube comes out of the abdomen on the right or left side of the body
- Controller: A small computer-like device that connects to the driveline and controls the function of the pumps. It also communicates information to the patient and the care team
- Power source: Battery packs or wall plugs are provided to help deliver power to the controller and pump.
Caring for Your VAD
The Loyola VAD team is dedicated to helping patients learn how to successfully live with their VAD and improve their quality of life. Patients receive extensive training and education on how to manage and care for their VAD, including how to troubleshoot any issue or emergency they may experience with the VAD.
Patients will have routine check-ups with their VAD team to monitor their post-VAD recovery and overall health and wellbeing. Your team may include:
- Advanced heart failure cardiologist
- VAD nurse coordinator
- Social worker
- Pharmacist
- Dietitian
The Loyola VAD team is here for you to make your experience as seamless as possible. We understand that you may be apprehensive about treatment. However, the entire Loyola Medicine VAD and cardiology teams are behind you, willing to do whatever it takes to make your treatment a success.
Our team has extensive experience working with patients just like yourself. The VAD program has been open and Medicare-approved since 2004 and has been a Joint commission certified program since 2013.
Meet Our Team
Featured VAD Videos
Father and Son Receive Heart Transplants 30 Years Apart
Grateful Father Blessed with the Gift of a New Heart
Locations

